Modeling protein release from affinity-based biomaterial delivery vehicles in spinal cord injury
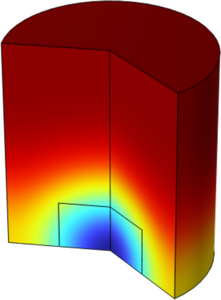
Spinal cord injury triggers an initial inflammatory response followed by scar tissue formation, hindering the repair of severed neural tracts and sensorimotor function.1 Injectable hydrogels consisting of a water-swollen polymer network can be engineered to mimic the environment of healthy neural tissue and serve as a minimally invasive platform for drug delivery. Hydrogels can be leveraged to release of a variety of therapeutic proteins to modulate the inflammatory response and promote neuronal regeneration across injured tissue.2–4 Despite their potential for regenerative medicine applications, the effectiveness of hydrogel platforms is limited by rapid burst release of loaded therapeutics, highlighting the need for greater temporal control over protein release and sustained delivery strategies. Hydrogel properties such as pore size, polymer molecular weight, swelling ratio, degradation rate, and binding affinity towards the drug have all been shown to influence the rate of therapeutic release. Previously, we have developed an in vitro one-dimensional protein diffusion model to determine protein diffusion coefficients within a given hydrogel matrix.5 We demonstrated that the diffusion coefficients of common proteins of different molecular weights, including bovine α-chymotrypsin (25 kDa), bovine serum albumin (66 kDa), and human immunoglobulin G (150 kDa), through collagen, alginate, and maleimide cross-linked poly(ethylene glycol) hydrogels could be accurately determined using this model. COMSOL Multiphysics software was then used to model the in vitro diffusion system and validate experimentally determined diffusion coefficients. Using the Transport of Diluted Species Physics module, we found no significant difference in the diffusion profile between in vitro and in silico models. Building upon this work, we have recently created a COMSOL Multiphysics model of injured spinal cord tissue with an implanted hydrogel to determine therapeutic protein release and retention profiles. The Hettiaratchi lab has previously designed affibodies, small protein-specific binders (~7 kDa), to control the delivery rate of target proteins from biomaterials.6 The binding affinity of the affibody to the target protein results from several thermodynamically favorable (hydrophobic, electrostatic, hydrogen bonding) interactions along the binding interface. Affibodies are incorporated into the in silico model to explore how varying protein-binder affinity interactions affect the hydrogel’s therapeutic release profile. Using the Optimization module, we will explore therapeutic design parameters, such as mesh size and polymer weight, to help identify hydrogel formulations best suited for controlled protein delivery. Through this in silico model of protein diffusion, we hope to provide a method for rapidly iterating hydrogel design, protein binder concentration and affinity, and therapeutic protein payload. Insight derived from this work will allow us to better predict protein diffusion kinetics in vivo and pave the way for more effective regenerative medicine strategies.